Your low-FODMAP diet needn't be low in fiber. Here are some good fiber sources suitable for a FODMAP-elimination diet:
Simple Ways to Help When Your Valentine Has IBS
How can I get enough calcium on a low FODMAP diet?
Q. How can I get enough calcium on a Low FODMAP diet? I am concerned about my bone health.
A. There are plenty of good sources of calcium on a low-FODMAP diet if you consume dairy products. If you avoid dairy for some non-FODMAP reason, you may not be able to achieve the recommended level of calcium intake without a supplement.
Calcium ReQuirements
Calcium is a mineral, and an essential building block for strong bones. Most of the calcium in your body is stored in your bones. Calcium also circulate in your blood, where it plays critical roles in muscle contraction, nerve signaling and blood clotting. The calcium level in your blood must therefore be very stable. Calcium is drawn from your bones when there isn’t enough calcium in your diet to maintain normal blood levels. Bone is living tissue that is continually being broken down and built back up. Osteoporosis occurs when the creation of new bone tissue doesn’t keep up with the loss of old bone. The bone mineral density of osteoporotic bones is low. Osteopenia is an early sign or stage of osteoporosis.
Your calcium needs depend on your age and sex. In the U.S. and Canada, recommended intakes are the same whether your bone density is normal or in the osteopenic or osteoporotic range. Adults up to age 50 should consume 1000 milligrams (mg) of calcium per day from a combination of food and supplements. Recommended intakes increase to 1200mg at age 51 for women and at age 70 for men. (Pre-teens and teenagers need more calcium, 1300mg per day.) Health authorities in some countries set lower targets for calcium intake. In the U.K, guidelines recommend intake of 700mg for most adults (1000mg for people on osteoporosis drug treatment), which might give you some comfort if you’re not able to achieve a higher intake.
What if I Don’t eat dairy? Can't I get the nutrients I need from other foods?
There is little chance of getting 1200mg of calcium per day from non-dairy foods unless you are committed to eating 1-3 servings of tofu daily along with small bone-in fish, tiny shell-on shrimps, and loads of greens, as many do in traditional Asian diets. Two full cups of fortified almond or rice milk every day would go a long way toward meeting your needs, but who does that? Most people choosing a dairy-free diet will need calcium supplements to meet their needs.
Good Low FODMAP Calcium sources
These foods are among the strongest sources of calcium in the low-FODMAP serving sizes suggested in the Monash FODMAP Diet App:
Firm tofu, as opposed to silken tofu, is a source of calcium because it is made with the naturally occurring coagulant calcium sulfate.
Lactose-free milk (300mg), lactose-free yogurt (180-290mg), lactose-free kefir (325mg), Cheddar cheese (300mg). sardines (400mg), calcium-fortified almond or rice milk (300-450mg), tofu (500mg), canned salmon, with bones (240mg), chia seeds (150mg), bok choi (75mg), corn tortillas (150mg), and sourdough bread (66mg).
The calcium from most other low FODMAP foods just doesn’t add up very fast. This can be due to the limited serving sizes, or because they just aren’t as rich in calcium as you may think. For example, the low-FODMAP serving size of kale, 1/2 cup raw, contributes just 12mg of calcium. Three-fourths (3/4) cup of broccoli has 30mg of calcium, one tenth the amount in a serving of yogurt. Low FODMAP servings of canned legumes (20mg) or almonds (30mg) are other minor contributors.
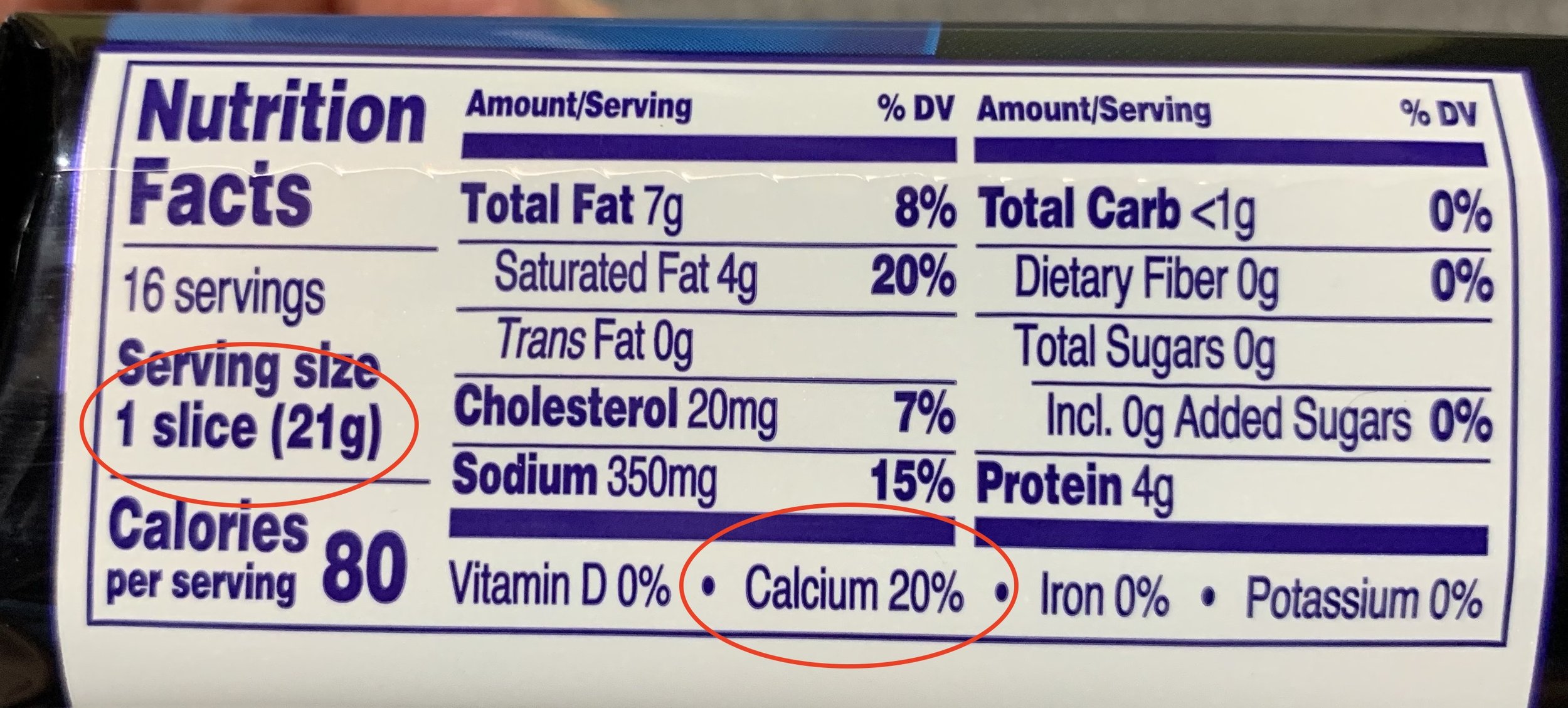
Label reading for calcium
The Daily Value (DV) for calcium is 1300mg. One serving of this food contains 20% of the DV, or 260mg (.20×1300=260).
Sometimes the Nutrition Facts panel spells out the amount of calcium in a serving of packaged food. In other cases you have to calculate it yourself, especially on small packages of food with limited space for details. Pay close attention to the serving size shown vs. the amount you actually eat or drink, and do the necessary math to calculate your intake. For example, a cup of lactose-free milk might well contain 300mg of calcium, but if you only put 1/8 cup of milk in your tea, you’ll be getting 37.5mg. (300÷8=37.5).
The target amount of nutrients used as a reference on Nutrition Fact panels is called the Daily Value, or DV. Why is the DV for calcium 1300mg? The DVs are not specific to any one age or gender. In this case, the reference amount of calcium selected for use as the DV was the higher amount recommended for older children and teens, rather than the 1000mg or 1200mg for adults.
Some foods don’t have Nutrition Facts panels, such as fresh fruits and vegetables. Sometimes you get lucky, and Google will present good quality data prominently on the page when it returns results for queries such as “how much calcium is in cheddar cheese”—look for the tag that says “Sources include: USDA”. If you have to dig deeper, look up the calcium content foods at USDA FoodData Central.
Estimate how much calcium you usually get from your diet. If you are short of the amount recommended for your age and sex, choose some of the good calcium sources suggested above to increase your intake on a consistent basis. Dairy products are ideal, because they come along with other nutrients, like protein, that are just as important for building bones, so choose them if you can. The best and most practical sources of calcium are foods that you could imagine yourself consuming every single day, such as adding one serving of lactose-free yogurt to your daily lunchbox.
Calcium Supplements
Not everyone has the option of getting calcium from milk products. If you can’t find a way to meet your calcium needs with food, ask the doctor who is treating your low bone density if you should make up the difference with a supplement. Practice guidelines for managing osteopenia and osteoporosis favor supplementation if, and only if, needed, but individuals with certain medical conditions shouldn’t take them without close medical supervision.
In all honesty, there are some unsettled questions about whether high-dose calcium supplements may be linked to heart disease or prostate cancer. You should balance these concerns against the real and present danger: you actually have a bone density problem right now, and you don’t want it to get worse. Until more is known about the possible risks, be conservative; avoid excess intake of calcium from supplements. Don’t supplement with calcium beyond your needs unless specifically prescribed by your provider. Many people find that a calcium supplement of around 400-500mg of calcium per day, together with some calcium from food, is enough.
To maximize absorption, take calcium supplements in divided doses, and choose a product that includes vitamin D. I usually recommend calcium citrate, because that form of calcium is well tolerated, can be taken with or without food, interacts with fewer medications, and is reasonably priced. It sometimes comes in “minis” or “petites” that make it easy to take 200mg twice daily. Calcium carbonate may seem attractive because it is cheaper, but some people find it causes bloating and constipation. (For this reason, don’t overdo Tums if you have IBS, because the main ingredient in Tums is calcium carbonate.) Ask your pharmacist if the calcium supplement you are considering will interact with any of your prescribed medications and when to take it to minimize interactions.
The information in the article is for educational purposes. If you need advice on your specific needs and how to meet them, consult the provider who is managing your bone health.
Further reading:
Calcium Fact Sheet for Consumers, National Institutes of Health Office of Dietary Supplements. Seen at: https://ods.od.nih.gov/pdf/factsheets/calcium-consumer.pdf Jan 16, 2025.
Morin SN, Feldman S, Funnell L, Giangregorio L, Kim S, McDonald-Blumer H, Santesso N, Ridout R, Ward W, Ashe MC, Bardai Z, Bartley J, Binkley N, Burrell S, Butt D, Cadarette SM, Cheung AM, Chilibeck P, Dunn S, Falk J, Frame H, Gittings W, Hayes K, Holmes C, Ioannidis G, Jaglal SB, Josse R, Khan AA, McIntyre V, Nash L, Negm A, Papaioannou A, Ponzano M, Rodrigues IB, Thabane L, Thomas CA, Tile L, Wark JD; Osteoporosis Canada 2023 Guideline Update Group. Clinical practice guideline for management of osteoporosis and fracture prevention in Canada: 2023 update. CMAJ. 2023 Oct 10;195(39):E1333-E1348. doi: 10.1503/cmaj.221647. PMID: 37816527; PMCID: PMC10610956, seen at https://pmc.ncbi.nlm.nih.gov/articles/PMC10610956/ Jan 16, 2025.
Protecting Bone Health Among Vegans, S Palmer, Today’s Dietitian 18 (2): 24, seen at https://www.todaysdietitian.com/newarchives/0216p24.shtml Jan 16, 2025.
This page may contain affiliate links. We are a participant in the Amazon Services LLC Associates Program, an affiliate advertising program designed to provide a means for us to earn fees by linking to Amazon.com and affiliated sites.
FODMAPs and Protein Powders
Smoothies: Easy Meals or FODMAP Bombs?
Smoothies have never been more popular! And why not? They taste great, can be assembled quickly, offer a convenient way to have a meal while on the job or in the car, and are a great vehicle for eating more fruits and vegetables. You can even use them to help you take nutritional supplements! As healthy as they can be, however, they are full of belly-ache potential.
Low-FODMAP Certification Programs
It would be lovely to have the time to make everything we eat from scratch, but few of us have the time or the inclination to do so. Even if you tend to think “processing” is a dirty word, be honest—when was the last time you made your own cheese, ground your own flour, or cracked the shells off your own nuts? So, we all need learn how to read food labels to determine which prepared foods are low in FODMAPs.
Is Sucralose OK on a Low-FODMAP Diet?
Is date sugar low FODMAP?
Q. Is date sugar low FODMAP? If so, in what quantities? I know dates are not, but I’ve seen conflicting information from low-FODMAP sources I usually trust and it’s not on the MONASH app.
A. The short answer: as of this writing, we can only guess about the FODMAP status of date sugar. It probably has a small low FODMAP serving size, less than 2 tablespoons.
Is date sugar low FODMAP?
Date sugar is made from ripe, pitted dates that are dried to a very low moisture content and ground into a powder. Dates are the fruits from certain types of palm trees. But date sugar is not the same as palm sugar, which is made from the sap of palm trees. The Monash University FODMAP lab has analyzed “dried dates” in general, and one specific variety (Medjool), but not date sugar, the packaged sweetener.
We see in the Monash University Low FODMAP app that somewhere between 1 and 5 dates, or .71 oz to 1.06 oz of dates are low FODMAP. It’s difficult to guess how this information equates to date sugar.
Dates vary in nutritional composition
There are hundreds of varieties of dates grown around the world. In Saudi Arabia alone, there are over 300 varieties of dates grown, and they vary significantly in sugar and moisture content. Other countries and regions have their own unique varieties of dates. The variety of date used isn’t usually specified by the manufacturers of date sugar, but the moist varieties meant for snacking on are not likely to be among them. Therefore, It isn’t likely that date sugar has the same FODMAP content as the dates that were analyzed for FODMAPs at Monash.
Serving size estimates
We don’t know how much moisture is lost, or how much the ground dates “fluff up” in the making of date sugar. So if we said, for the sake of argument, that the type of sugar was similar to the dates in the app, we would have to figure many teaspoons or tablespoons of date sugar would equal the amount of FODMAPs in 1 pitted date. My calculations suggest that 2 tablespoons of date sugar has about the same amount of total sugar as one Medjool date.
Effects of ripening and drying
Adding more uncertainty, the final stages of ripening and drying of foods can alter their FODMAP content in unpredictable ways (check out the difference between grapes and raisins, or rice and puffed rice). As dates ripen, much of the sucrose content is “inverted”, or broken down to glucose plus fructose. Does that continue or change during the further drying of dates for grinding? It’s anyone’s guess. To be on the safe side, my guess will be conservative. Pending actual lab analysis of date sugar, less than 2 tablespoons might be low in FODMAPs. Larger servings might be a significant source of sorbitol and fructans.
Conclusion
Like many foods, dried dates can actually be low, medium, or high in FODMAPs depending on the serving size. Dates meant for eating have been lab tested, but date sugar has not. If you’d like to bake with date sugar on your low FODMAP diet, my advice is to make sure there’s less than 2 tablespoons in your portion of the recipe.
Further reading:
AlShwyeh H, Almahasheer H. Glucose content of 35 Saudi Arabian date fruits (phoenix dactylifera L.), Journal of the Saudi Society of Agricultural Sciences 21 (2022) 420-424. Seen at: https://www.sciencedirect.com/science/article/pii/S1658077X21001545
Why Not Stay Low FODMAP Indefinitely?
Q. After going low FODMAP a few years ago, I’m still loosely eating that way. I’ve read it is not good to stay on the diet long term but I feel like it really helps me keep IBS undER Control. Why not stay low FODMAP INDEFINITELY when it may be helping?
The short answer is that a Low FODMAP diet may be too limited in some cases. More variety, usually results in a more nutritious diet and promotes a better food quality of life.
In many ways it is so much simpler to just follow the rules and stay low-FODMAP than it is to go through the uncertainly of the reintroduction process. But simple isn’t always easy, is it? In fact, most of my practice these days, almost 15 years into the FODMAP era, consists of helping people take those next important steps toward a varied diet. Why bother?
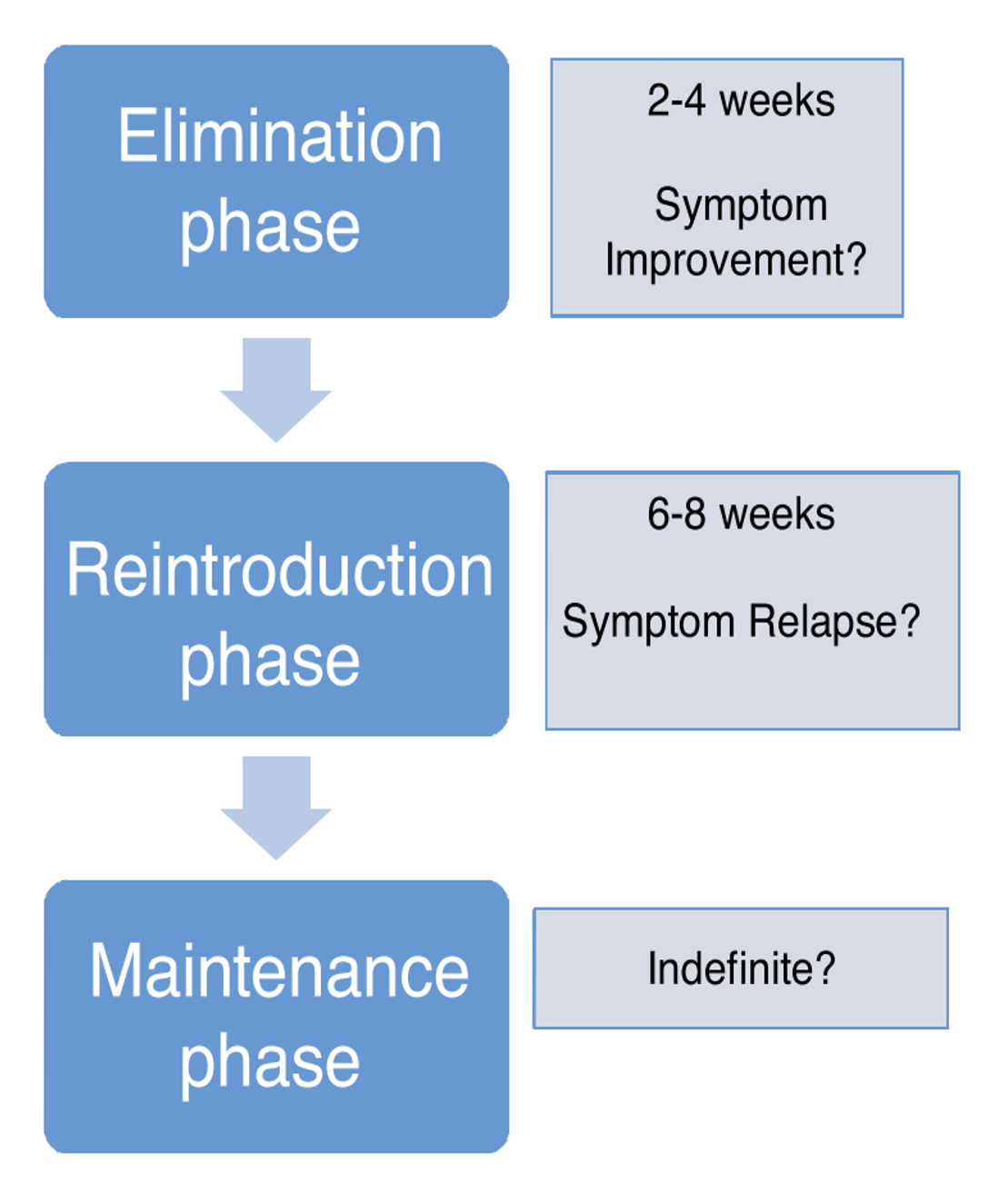
Ideally, the FODMAP elimination diet is a short dietary experiment. Eswaran SL Curr Opin Pharmacol, 2017
As you have read, low-FODMAP diet is meant to be a short dietary experiement, to get IBS symptoms under control. If it doesn’t work for you, don’t continue it. If it does improve your abdominal and bowel symptoms, it should be followed by a reintroduction process. That is the only way to figure out which FODMAPs are (and are not) symptom triggers for YOU. They are not the same for everyone. This paves the way for you to enjoy a more varied diet.
A Varied Diet is more nutritious
Fortunately, there are good low-FODMAP sources of all nutrients. So if you are willing and able to eat a wide variety of low-FODMAP foods you might not have to worry too much about this one. But, if you add other dietary restrictions, you can find yourself eating a repetitive, short list of foods that comes up short in some areas. For example, it can be difficult for vegans to get enough protein on low-FODMAP diets, if they are used to eating a lot more beans, nuts and seeds. Other people might be at risk for poor intake of certain nutrients even on their usual diets, in ways that have less to do specifically with FODMAPs. For example, people on dairy-free diet rarely get the recommended amounts of calcium from food. People who don’t care for green leafy vegetables or nuts probably aren’t consuming enough magnesium, and so on.
Some FODMAPs are important prebiotics
Fructans and GOS are two of the six FODMAPs that are limited on low-FODMAP diets. They are also well-known prebiotics. Prebiotics are selectively fermented by the “good” bacteria in you gut, to produce beneficial substances like short chain fatty acids. When you are on a low-FODMAP diet you cut back on these a great deal.. Hopefully you are still eating low-FODMAP servings of foods that contain some fructans and GOS, along with good low-FODMAP sources of prebiotics. Choose low-FODMAP servings of whole grains, fruits, vegetables, nuts, seeds, and legumes. After the reintroduction process, you should eat larger servings of these foods if you can tolerate them, to increase your intake of prebiotics.
Food Quality of Life
Sharing is an important part of “food quality of life”. Photo credit: C. Catsos
Most people find that their food quality of life is better when they are eating a more varied diet. What does this mean? It means being able to share in communal food life and (mostly) eating what is served when dining with friends and family. It means not having to say “no” to everything just because you are following the rules, and not having to bring your own meals to gatherings. It means enjoying occasional restaurant meals with more confidence. It means generally just having a better relationship with food and being less afraid of food and eating.
Be Sure
Your question indicated you “feel like” low FODMAP diet keeps your IBS under control and “may be helping”. You need to be more certain than that to justify the potential drawbacks of a long term low FODMAP diet. Self-knowledge is your ticket forward. Gain it by reintroducing FODMAPs in a structured way, monitoring symptoms, then adjusting your diet as tolerated.
This page may contain affiliate links. We are a participant in the Amazon Services LLC Associates Program, an affiliate advertising program designed to provide a means for us to earn fees by linking to Amazon.com and affiliated sites.
Is It Possible to Reintegrate Problem High-FODMAP Foods?
Q. I’ve been on the low-FODMAP diet for at least 7 years. I’ve consulted 3 doctors and one nutritionist, and no one has been able to enlighten me as to whether it’s possible to reintegrate the problem foods. You seem to say that it is possible. Can you kindly elaborate on how one does this? If there’s a way to condition my body to accept higher-FODMAP foods I would love to know about it.
Short Answer: For most people with IBS, it’s possible (and recommended) to at least partially reintegrate some high-FODMAP foods. Which foods (and how much) you will be able to reintegrate is revealed through careful observation during the reintroduction phase of the diet program. The reintroduction process is less about conditioning your body to accept high-FODMAP foods, and more about learning what your limits are. Being able to eat an overall high-FODMAP diet in the future is not one of the expected outcomes of the FODMAP elimination and reintroduction process.